At Long Island Spine Rehabilitation Medicine, our doctors are highly regarded for their successful treatment of all types of joint pain, including back and leg pain that results from spondylolysis and spondylolisthesis. As well-credentialed physiatrists (physicians who specialize in pain management and rehabilitation), we are fully prepared to provide pain relief and improved function to our patients. It is estimated that 5 to 10 percent of people with back pain are suffering from one or both of the conditions mentioned. African Americans seem to be at greater risk.
What is spondylolysis? What is spondylolisthesis?
Spondylolysis is a stress fracture in one of the vertebrae (the bones that compose the spine).
When spondylolysis weakens the affected bone so much that it can no longer maintain its proper position in the spine and slips out of place, the condition is known as spondylolisthesis.
These conditions typically occur in children and adolescents who engage in sports that stress the lower back, such as football, gymnastics, wrestling and weight lifting, but can also occur in adults as a result of the wear and tear of aging and arthritis. In most cases, if patients rest and take a break from all strenuous activities for a period of time, our physiatrists and spondylolysis and spondylolisthesis physical therapists are able to greatly improve their conditions with noninvasive, conservative methods of treatment.
When Spondylolisthesis Requires Surgery
There are cases in which this condition causes persistent back pain, having resulted in severe vertebral slippage. Some individuals develop a fracture that does not heal completely due to repetitive stress and excessive weight-bearing.
Occasionally, this will ultimately cause a break between the front and back of one of the lower vertebrae. In such a situation, surgical intervention may be necessary. If this is so in your case, we will refer you to colleagues with excellent surgical skills for your operation and be ready to assist you in rehabilitation after you undergo the procedure.
What are the symptoms of spondylolysis and spondylolisthesis?
Patients who suffer from this type of fracture in the lower back may experience one or several of the following symptoms:
- Pain when leaning back or extending the lumbar spine
- Low back pain
- Buttock pain
- Radiating pain, numbness, tingling, or weakness in the legs
It’s important to realize, however, that these pains may appear years after the original injury due to a secondary condition. The patient’s spinal nerves may be impinged on by mechanical pressure due to a narrowed spinal column (spinal stenosis), disc degeneration, arthritis or cysts of the facet joints between adjacent vertebrae — any of which may have been caused by the initial fracture.
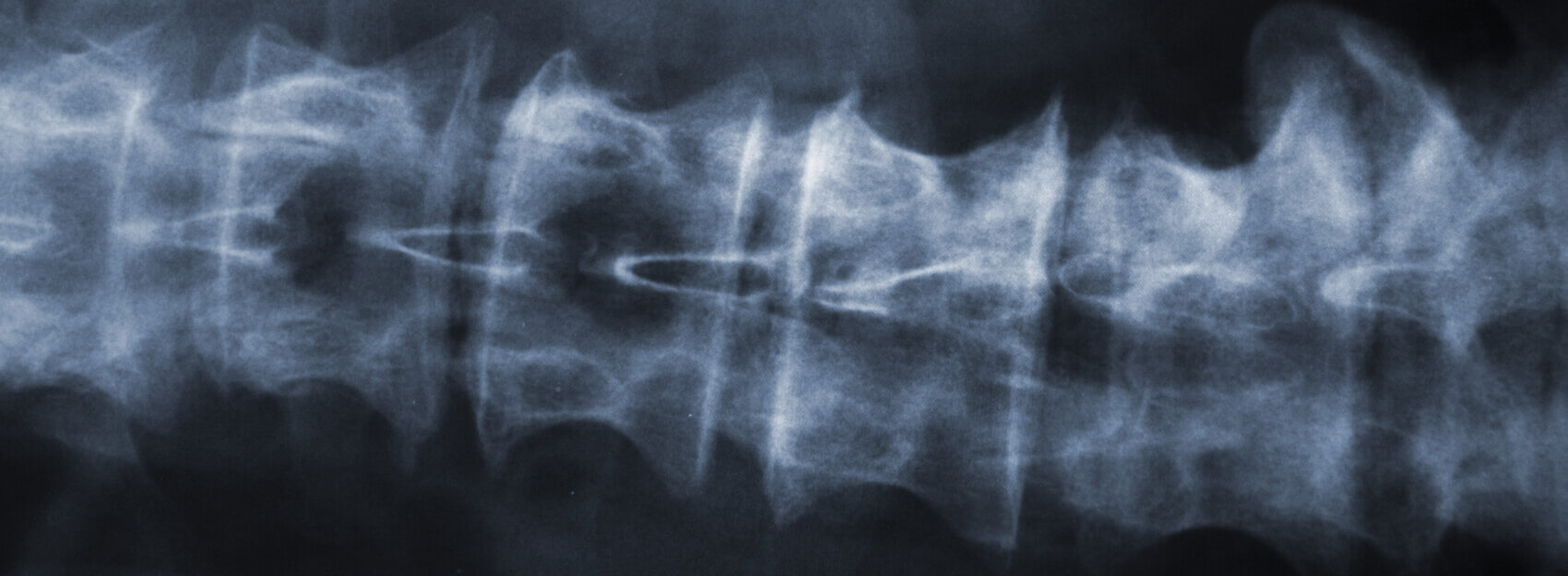
How We Diagnose Spondylolysis or Spondylolisthesis
Because patients with the small fractures of spondylolysis are sometimes asymptomatic, the fact that we see one on your X-ray does not mean it is the cause of your pain. For this reason, our doctors take great care to make a definitive diagnosis by:
- Taking a complete medical history
- Examining your X-rays very carefully
- Ordering other diagnostic tests — CT, MRI scan or more rarely, bone (SPECT) scan — if necessary
The use of MRI imaging has allowed us to confirm the vast majority of such cases without the need for bone scan imaging which is associated with higher degrees of radiation exposure for the patient.
Spondylolysis Treatment/Spondylolisthesis treatment
At Long Island Spine, we always begin with the most conservative treatments we feel will be effective in relieving your pain and restoring your mobility. For our younger patients, we typically prescribe rest and temporary disengagement from sports in order to allow the fracture time to heal. Many of our young patients are also fitted with a customized back brace to prevent further damage and promote healing.
Physical Therapy for Spondylolysis and Spondylolisthesis
Our talented physical therapists are extremely knowledgeable about how to treat disorders of the spine, including spondylolysis and spondylolisthesis. We are also aware of how eager most young patients are to begin participating in their sport of choice again. Therefore, we will gradually begin to involve patients in a spondylolysis physical therapy program that is sport-specific as soon as their pain has subsided enough for such activity to be safe.
Customized exercises will help them to strengthen the muscles they need to protect their spine from further injury. Our goal is pain reduction and increase of strength and flexibility.
We will also address the back and leg symptoms that usually accompany spondylolysis and spondylolisthesis by guiding patients through flexion-based physical therapy. This type of physical therapy is based on the premise that stretches and other exercises work best when they follow the body’s own natural desire for comfort. In other words, we help you to work out in positions and postures that feel most pleasant and beneficial. We will also work with you to compile a home exercise program to help you maintain your renewed strength and stability.
Medication Management
Our empathic physiatrists know all too well how debilitating pain can be and how it can be counterproductive by interfering with physical therapy exercises. Therefore, we recommend correct dosages of over-the-counter painkillers to lessen or eliminate our patients’ pain. If pain is severe or intractable, we may prescribe stronger analgesics for a brief period of time. We may also prescribe muscle relaxants to assist in pain management.
At Long Island Spine, we are careful to keep dosage levels as low as possible to maximize benefits while minimizing uncomfortable side effects, such as drowsiness and constipation.
Interventional Procedures
If you present with severe back or leg pain due to spondylolysis or spondylolisthesis, we may also administer epidural injections that target the affected spinal nerve or facet joint. The injections will contain a mixture of a corticosteroid and a local anesthetic to address issues of both inflammation and pain. By administering these injections under fluoroscopic guidance we can be confident of a high degree of precision.
Another interventional procedure we frequently use is acupuncture. Studies have shown that both spinal injection procedures and acupuncture have proven effective in cases in which other treatment options failed. It should be noted that we administer acupuncture only in our East Meadow and Great Neck offices.
Contact Long Island Spine and Start Feeling Better
Our exceptional doctors are here to reduce your pain and improve your activity level. Don’t let your condition get you down — no matter how difficult it is to spell or pronounce. If you are suffering with spondylolysis or spondylolisthesis contact us promptly so we can help you restart your life.